A load of Turkish irony
Turkey joining the EU wasn’t a scare tactic used to promote Brexit, was it?
No, I didn’t think it was. That would lend itself too easily to satire, when an RAF plane loaded with personal protective equipment from Turkey has been failing to reach the UK on a daily basis for half of the past week.
Another eventful day in the level 1 Covid-19 zone. Inconsistencies in social distancing by workplace colleagues have been matched in dark entertainment value by the sheer variety of ways in which PPE has been repurposed. A hard-earned al fresco lunch break in the lockdown-special spring sunshine, sandwiches clutched in gloved hands. A used FFP3 respirator mask safely stored on a colleague’s work-desk, nestled between clinic letters and his coffee mug. Fluid resistant surgical masks warming one’s chin, or dangling a new trend in ear wear. You could be excused for thinking - aha! this must be what the health secretary meant by suggesting the NHS should use PPE appropriately, yes?
The truth of this matter is embarrassing, and it is not healthcare staff that it casts in a poor light. Every one of these workers is clinging on to their PPE because there isn’t enough to go around. The porter opening the ward doors in her gloved hands; the nurse finally managing to grab a cup of tea, his mask lining the palm in which he rests his chin; the medical student bustling about the entire so-called-green ward area all day in the same skimpy plastic apron. Each one of them dares not dispose of their mask, glove or apron. There isn’t enough to go around. There might be no gloves or gowns available in an emergency to resuscitate a patient. Extraordinarily, some managers have even told staff there is a strict limit on how many pieces they are allowed during one shift.
This is a lose-lose situation. The paucity of PPE is causing healthcare staff to keep wearing the same items in a way that does more harm than good. Thus, the porter heads down the stairs, burnishing the banisters with a variety of bugs, coronavirus included, from her gloves. The nurse smears his own face with all manner of organisms trapped on the mask he has continued sort-of-wearing as he sips his now lukewarm tea. The student’s apron makes sure that the covid-positive patients who are invariably present on the “green-zone” wards - because we still are not testing comprehensively - have every chance of sharing their infection with those yet to contract it. The only thing gained from this desperate use of undersupplied PPE is a misplaced sense of false security. In reality, this manner of make-do usage protects neither carers nor the community.
The ironic grain of truth in the health secretary’s scurrilous insinuation is that health workers are struggling to use PPE appropriately, as in, safely. We cannot retain the same items of PPE across multiple patient interactions; such usage will cross-infect our patients and fail to protect us. A reliable and adequate supply of personal protective equipment for healthcare staff is an inarguable necessity; providing it is a responsibility the government cannot wash their hands of.
Live in the time of Corona - this is HOW you do it
Personal suggestions from a frontline clinician
I am a consultant vascular surgeon employed by the NHS in a full time clinical role. We, as a specialty, have markedly altered our working practice to help care for covid-19 patients. The comments below reflect my personal views, based on my interpretation of available scientific facts and official guidance from international bodies. Please read, interpret and apply based upon your own judgement, taking local and governmental instructions and policy into account.
A related blog on this website details my reasons for putting these tips out for the public.
1. The Golden Rule - maintain a 2 metre distance.
This is the single most important precept. Do not be closer than a 2 metre distance with anyone that you don’t live with. If you can’t tell what 2 metres is, as I read on a Twitter feed, imagine a 6 foot tall person, wearing a hat and boots, lying stretched on the floor between you and the person you are about to interact with.
Most of the contagion of Covid-19 is through droplets from infected persons. This will come off the person from their mouth as they speak, from their nose as they exhale and will obviously be contained in any sneezes or coughs. The person does not need to have symptoms, to be infectious. More than 50% of spread of this viral infection originates from asymptomatic persons - those who are not ill at the time.
If you are exerting physically, such as running or exercising hard, you should probably double your safety distance to 4m. My rationale is that your breath stream will travel that much more / you will inhale that much more, during such activity. I will look for any evidence about this and update in due course.
2. Beware the fomites.
Fomites are inanimate objects that can transmit infections. These include numerous items of our modern existence - phone handsets in the hospital; your own mobile phones; your keys; door handles; elevator buttons; microwave doors; fridge surfaces; your dog’s collar; the list is obviously interminable.
It is impracticable to be cleaning all of these all the time. The principle I am adopting therefore, is to maintain your individual safe environment, and to be on constant alert when you are outside of it. This should be relatively easy for those of us staying at home, and slightly harder for those who must go out to work. It is very do-able, nonetheless. Here is how I go about it :
- When I enter a new environment, such as my vascular surgery office in the hospital, I wipe down and clean all the surfaces I need to be in contact with; the mouse, mousepad, computer keyboard, desk surface, top of folders. It is impracticable to wipe all the paper so I treat these as non-clean.
- I do the same on a daily / 48 / 72 hour basis for the relevant items at home, depending on how much each fomite has been touched.
- I minimise contact with all objects outside of my ‘safe zones’; my home and my immediate work environment.
It goes without saying that hand hygiene remains of paramount importance. Taking off outerwear, and then thoroughly washing your hands with soapy water is vital. This must be done before you set about cleaning all the above surfaces, for the process to be effective.
3. Don’t eat coronavirus.
This seems obvious, but is easily overlooked. The maxim of ‘avoid touching your face’ is a tough one at the best of times. It is obviously almost impossible to avoid your hands being close to your face when you eat. Thus, it is crucial to never eat without cleaning your hands fully. Are you going to eat outside your home, in your workplace, for instance? If so, make sure your hands are clean, and do not handle any objects during your meal that might be infected. This would include things like paperwork. The covid-19 virus can survive for varying lengths of time on almost all inanimate (non-living) surfaces.
4. Maintain your immunity and your mental health.
I am taking a multivitamin supplement on a daily basis, as are all members of my family. Many of us are deficient ‘normally’ in trace minerals that are important for immunity, such as Zinc, Magnesium, Selenium. A multivitamin that tops up all of these is likely to keep your immunity high. Other contributors to a good immune response are eating and sleeping well.
Recognise that the stress of the lockdown, of going to work in these circumstances and of the lack of social contact can all ‘get you down’. Find your own ways to address this before it becomes a bigger problem. There is plenty of help online. I will put links on as and when I verify them.
5. Follow Social Media.
I cannot overemphasise the value of this. Mainstream media (MSM) are letting themselves down deplorably during this pandemic. I stopped trusting The News on the day that an official 1 million strong (at least - the real figures are thought to be higher) public rally in support of the junior doctors’ strike in 2015 did not make the hourly news on many flagship radio stations and TV, and barely featured in newspapers. I do not understand why MSM in a country like the UK does not hold authority properly to account. After a day when more than 900 people in the UK died of coronavirus (Maundy Thursday 2020), some tabloids led their front pages with the statement that it was a Good Friday because the Prime Minister was sitting up in bed.
I use Twitter. I don’t use Facebook, but you should find whatever works for you. My general impression is that Twitter has better ways of filtering out fake news than FB, but I can’t state this with authority as I do not use FB. An adage I have heard is “Twitter is where you tell the truth to strangers, and FB is where you lie to your friends”.
Twitter is easy to create a new account on, free to use, and quick to browse. If you put in a hashtag, you can find all the information you want about any topic. You could search for #covid19, or #PPE or #LoveInTheTimeOfCholera. It all works.
Once you get on Twitter, find people who seem to tweet things you find useful or like reading, and ‘follow’ them so that your Twitter timeline is automatically populated with their wisdom or folly. My twitter handle is @bloodysurgeon and my therapy dog Saoirse’s is @bloodydoggy.
6. PPE for the public.
Finally. The burning question. Should we use masks in public, and all the related queries. I will come back to this with references as soon as I can. For now, my personal opinion - and I stress, this is my suggestion, my advice, my recommendation, not (yet; one lives in hope!) official guidance - is very simple:
Follow rule 1 [keep a 2m distance from everyone you don’t live with]. This includes key workers in their offices, factories and hospitals. There is no logic in following social distancing at home and then flaunting it at work.
If you cannot follow rule 1, then cover your face.
Covering one’s face has two objectives:
[1] cover your own nose and mouth, with a cloth, fabric or paper mask, in order to minimise the risk you will give the virus to another person*
[2] shield your eyes, along with your own nose and mouth, to minimise the risk of you getting the virus from another person.
Your unprotected eyes are much more exposed constantly (while you are awake) compared to your closed nose and mouth. It follows therefore - if you need PPE for your face, it makes sense to include eye protection.
The single most important aspect of using PPE on your face is this : do not do more harm than good.
Follow good technique for the use of PPE:
Make sure the PPE item is clean before it goes on your face.
Do not touch your PPE while you are wearing it.
Use it for a limited time during an encounter where you cannot maintain Rule No. 1.
As soon as you can, remove the PPE safely, touching the outer surfaces as little as possible, clean it, and put it away safely.
Now, clean your hands, all the way up to your forearms beyond your wrists, using soap and water, ensuring that you’ve created a healthy lather of soap bubbles before you wash away those killed covid-19 bugs.
Repeat as needed.
*There are online resources for making your own masks safely, and for cleaning them. I will put links on as and when I am able to verify them.
Good luck, everyone.
Stay safe, stay strong, stay sensible.
laugh at one #covidiot A day and we’ll get through this.
Live in the time of Corona - the WHY section
Why, as a frontline clinician, am I offering personal suggestions about Covid-19 safety tips?
Official guidance about Coronavirus 2019-20 from national governments and public health bodies has altered many times. This is understandable, in light of the rapid progression of a new virus across the globe.
UK guidance has taken longer to take shape or become effective, than many consider reasonable. This perception of delay or inadequacy is based on a comparison with actions taken by other similarly affected countries, a disparity with @WHO guidance, and a logical interpretation of available facts and science.
I have prepared this set of suggestions for the reason above. I am not writing these as part of my clinical role, which remains subject to policy from Public Health England (@PHE_uk) as well as that at my employing NHS Trust. My twitter timeline on @bloodysurgeon charts the ongoing difficulties both public and professionals continue to raise daily regarding aspects of the UK’s covid-19 response. These include lack of sufficient testing of NHS staff, lack of contact tracing, absence of an antibody test… and most importantly, scarcity, confusion and general dissatisfaction with regards to personal protective equipment (PPE). None of these are trivialities. The lack of testing means that we do not know who among colleagues is symptomatic; the science says more than 50% of spread of coronavirus-SARS-Cov-2 originates from people without any symptoms, i.e., those who are clinically well and who are at work, including in primary and secondary healthcare settings. The absence of contract tracing means we cannot realistically hope to get a firm grip on the epidemiological spread of the disease - it will reduce our current lockdown, in my opinion, to a sticking plaster that will come off and reveal that we have done very little to tackle the cause of the underlying wound. Without an antibody test, we cannot determine which persons who already recovered from Covid-19 are now most safe to take on the highest risk exposures in treating severely ill coronavirus patients.
The last point is particularly germane in light of the ongoing PPE difficulties. I will write a separate piece about PPE, but evidence of the nature and scale of the problem is all over social media for you to inform yourself.
At an individual level, I have advised my immediate family, friends and neighbours from early March 2020 about #covid19 safety measures. In light of our current coronavirus strategy, I feel it appropriate to share my suggestions with the general public. These are recommendations intended to increase your own safety, that of your family, and that of your community. Please read, interpret and apply them according to your own judgement. Please recognise that these are my personal views rather than those of the organisations I work for, or societies and bodies of which I am a member.
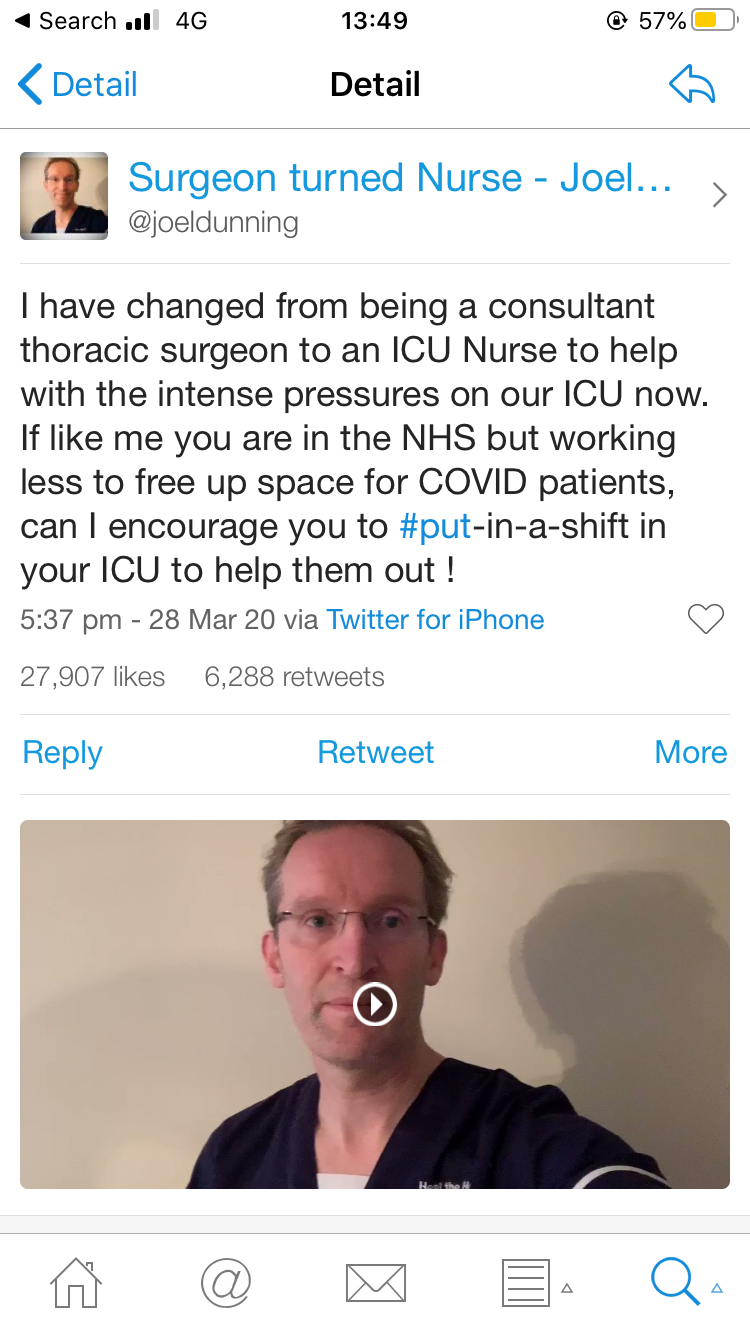
#Put-In-A-Shift
Redeploy yourselves to ICU if there’s a felt need you can address
This is a tweet from Thoracic surgeon in Middlesborough, Joel Denning.
#SocialDistancing
This is a twitter post by @ZhangJielai. She’s not sure who came up with it. It is a brilliant illustration of the power of social distancing to flatten the mortality curve of Covid 19, compared to efforts based only by healthcare teams.
#LowerTheBaseline
https://twitter.com/EpiEllie/status/1243948802660278272?s=20
From @EpiEllie
Along with efforts to #FlattenTheCurve, she says, let’s #LowerTheBaseline.
Let’s all be sensible and reduce the load on the NHS to the absolute unavoidable minimum. We will be stretched beyond capacity by the Covid19 pneumonia caseload. We need to work together to save lives.
A viral iteration of Work-Life balance
https://www.theguardian.com/world/2020/mar/25/dispatches-from-the-covid-19-frontline
Stay on the sofa. Save the world.
A tweet from Phyllis Fagell @Pfagell, uncredited
https://twitter.com/Pfagell/status/1244026645415157760?s=20
We Must Create Breathing Space
Letter to the Guardian (unpublished) dated 15th March 2020
I grimly acknowledge our vulnerability to Covid-19 as described by a fellow NHS consultant to Denis Campbell in today’s Observer. [NHS frontline: One doctor’s story, 15th March 2020]. Incessant defunding and the crippling of community health services mean that nurses and doctors have been functioning in crisis mode day and night for over a decade. Sadly (and in an undeserving reprieve for some), efforts to mitigate this imminent catastrophe must take precedence over answers and accountability.
It is imperative that each clinical specialty mobilises their available resources towards the most serious complications of Coronavirus infection. Care for patients in mine (vascular surgery) is broadly categorised into three groups: (1) ‘elective’ - cannot walk far due to chronic arterial disease, (2) ‘urgent’ - severe arterial narrowings that cause constant pain, and (3) ‘emergent’ - abrupt and total disruption of blood flow. I recommend that we defer the first indefinitely, prioritise the second at consultant discretion on an individual patient basis, and maintain the third as best we can.
Cases of lethal pneumonia from this pandemic will decimate the reserves of NHS respiratory care. Every other department must sharply redefine job roles and redeploy to the need of the hour. We must reallocate operating theatre ventilatory equipment, provide crash-training so that other specialty colleagues can assist the intensive care teams, and reorganise work rotas sensibly to minimise staff morbidity and mortality. Organisational leadership must empower us to do so. There is no more time to lose.