POVS on CLTI - Marcus Brooks
Marcus Brooks for the VS on Provision of Vascular Services document 2019 being formalised into NHS CQUIN 2022/23
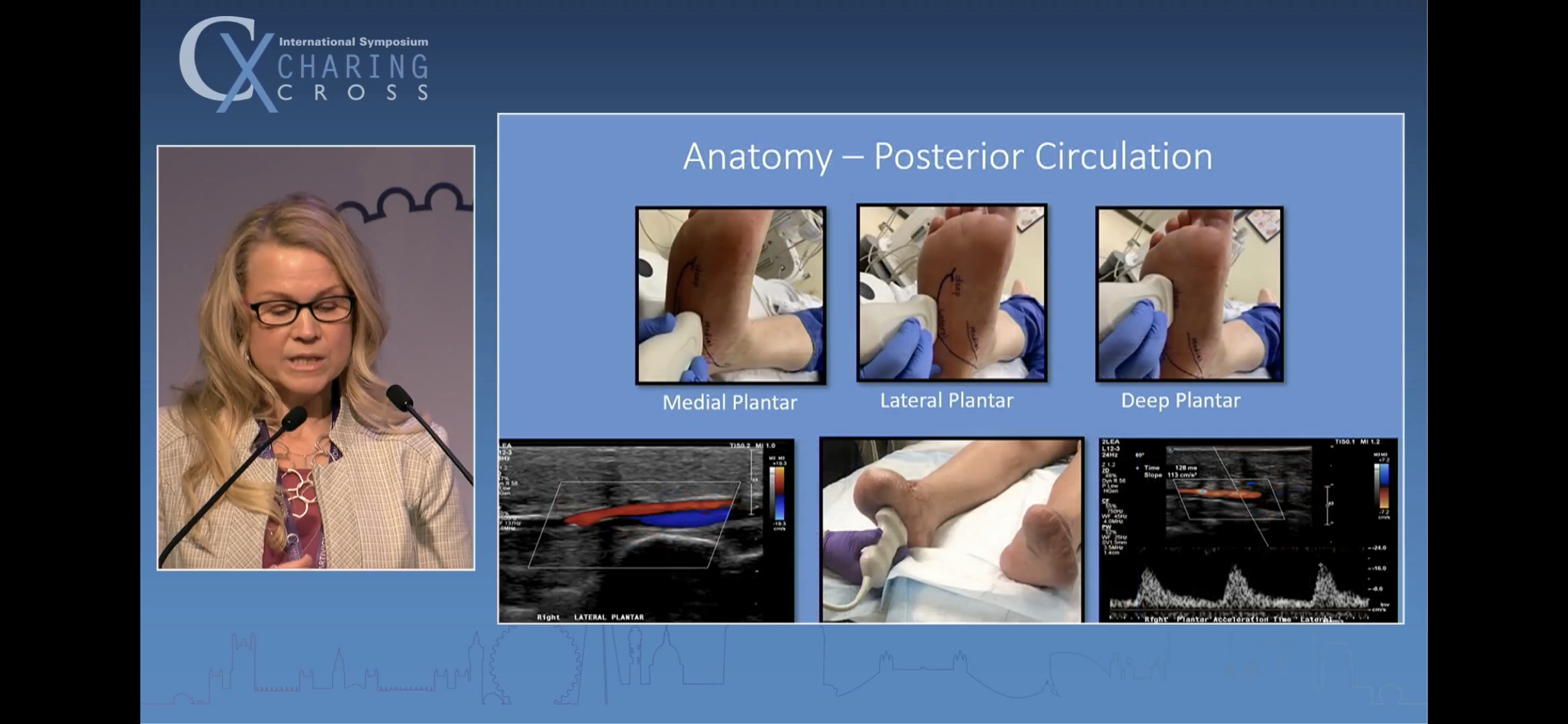
Plantar Acceleration Duplex
Talk by vascular scientist in the USA - using acceleration time on duplex to grade plantar blood flow.
Jill says primary objective is understanding whether a foot that is in trouble is ‘hibernating’ or ‘desert’. Well put.
Helpful description of the named arterial branches beyond the ankle level. They use either a conventional linear or a hockey stick probe.
The metric is time taken for the arterial pulse to progress from onset to peak of systole. Lower, the better.
I’ve looked up the abstract of Jill’s original 2019 paper below. The time metric is milliseconds (ms). They grouped patients in 4 classes based on clinical symptoms + ABI, class 1 being normal and 4 being rest pain/ tissue loss.
I am representing their paper conclusions as below: Normal foot: PAT 1-120 msSlightly ichaemic foot: PAT 121-180 msModerately ischaemic foot: PAT 181 - 224 msThreatened severely ischaemic foot: PAT over 225 msPedal puncture case - Mariano Palena, Abano Terme
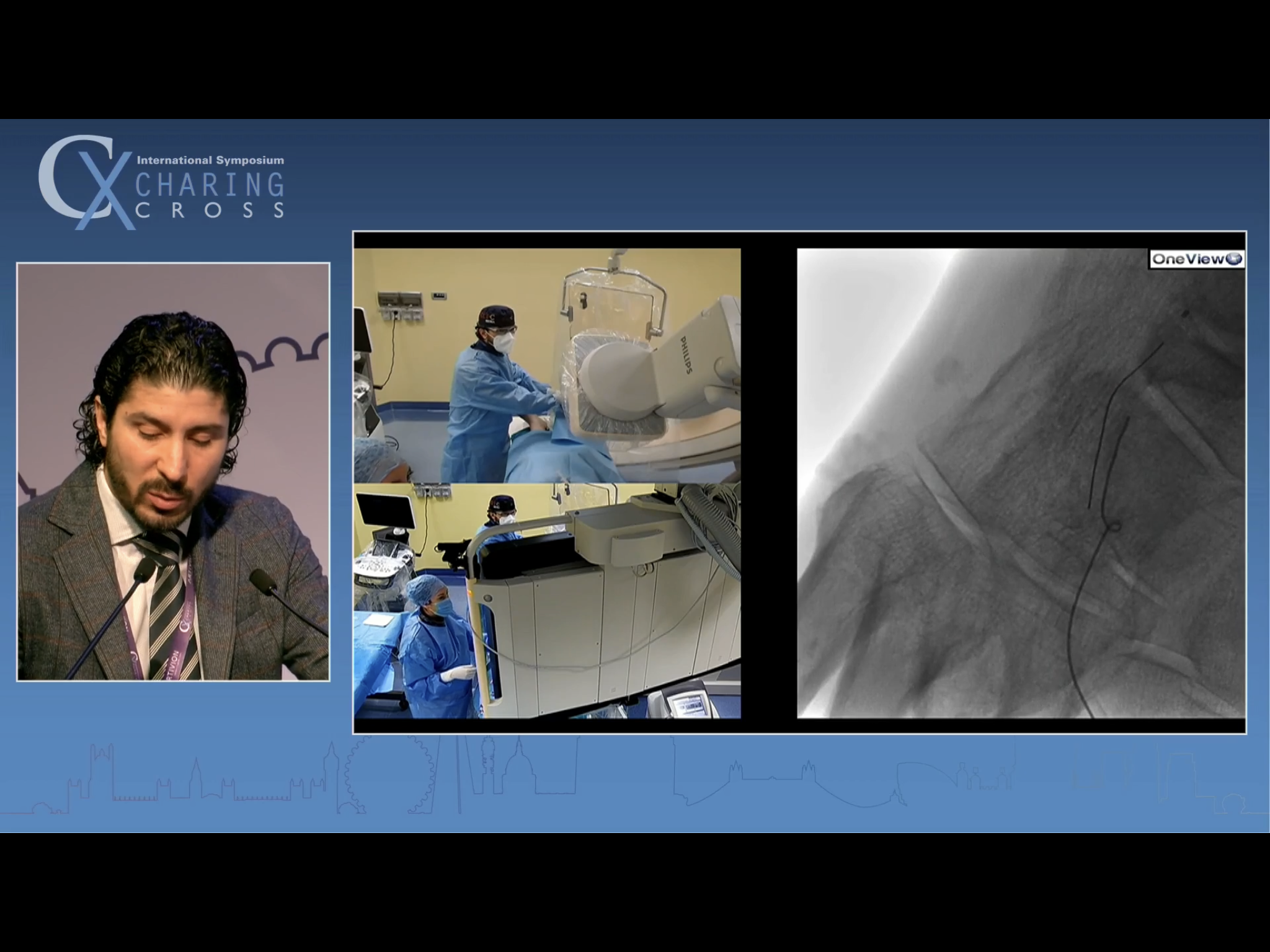
Dr Marco Manzi’s protege presents a talk on CTO technique in very distal BTK CLTI
He says he is using CO2 to minimise contrast load. At the end of the talk he was asked how long these cases take. He said usually 1-2 hours. Said he tries not to go over 2 hours, as he finds that that is when the awake patients lose patience.
The antegrade approach wire is refusing to track down the calcified DPA
Fluoro (and calcium) guided puncture into an arterial branch in the 1st web space
Clearly apparent from the distal (luminal) wire that the retrograde puncture was necessary - the proximal wire has tracked away from the target vessel
manipulation of the retrograde puncture wire into the distal ATA
Capturing the retro wire into the antegrade catheter to achieve through and through access
Retaining the distal wire provides pulsion + traction to get the balloon through into the DPA. He eventually used a 2.5 mm balloon in the DPA. Schneider commented on it. Palena said it was a large vessel.
Having got through, seeking to improve as much of the pedal arch as possible and to get through the loop
I’m afraid I missed capturing the lateral foot run he showed, which looks more impressive than this AP shot.
Ultrasound screening of the Angioseal deployment. I asked if this was standard practice in his unit. He said yes, and said it was a ‘matter of school’. When he started in the unit, Manzi said he could do whatever he wanted, but he must use U/S going in and U/S coming out. So he does.
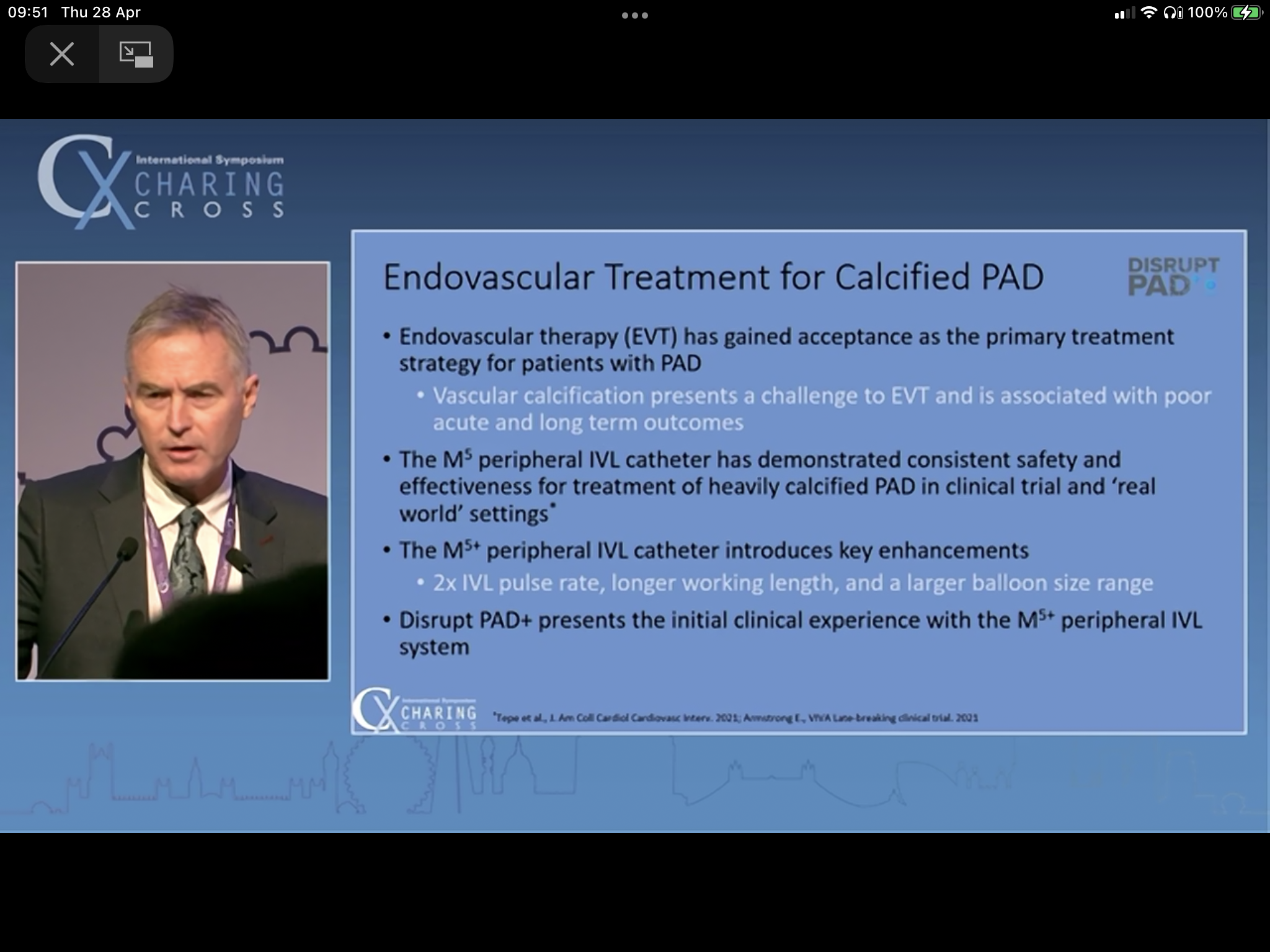
Lithotripsy in CLTI - Andrew Holden
Holden championing value of lithotripsy for calcified BTK CLTI disease. In brief.
main thrust of talk related to new catheter having an 8mm diameter option, meaning CFA and iliac are treatable.
Debus on DOAC after revasc.
Prof Debus, ex ESVS president, summarises role of DOAC therapy post revascularisation
Debus states that neither the use of single or dual antiplatelets, nor full anticoagulation, was found on clinical research to substantially improve limb or mortality outcomes post revascularisation
COMPASS trial was stopped early because the benefit seen in preventing MACE was substantial (26%). The truncation stimulated set up of the VOYAGER PAD trial.
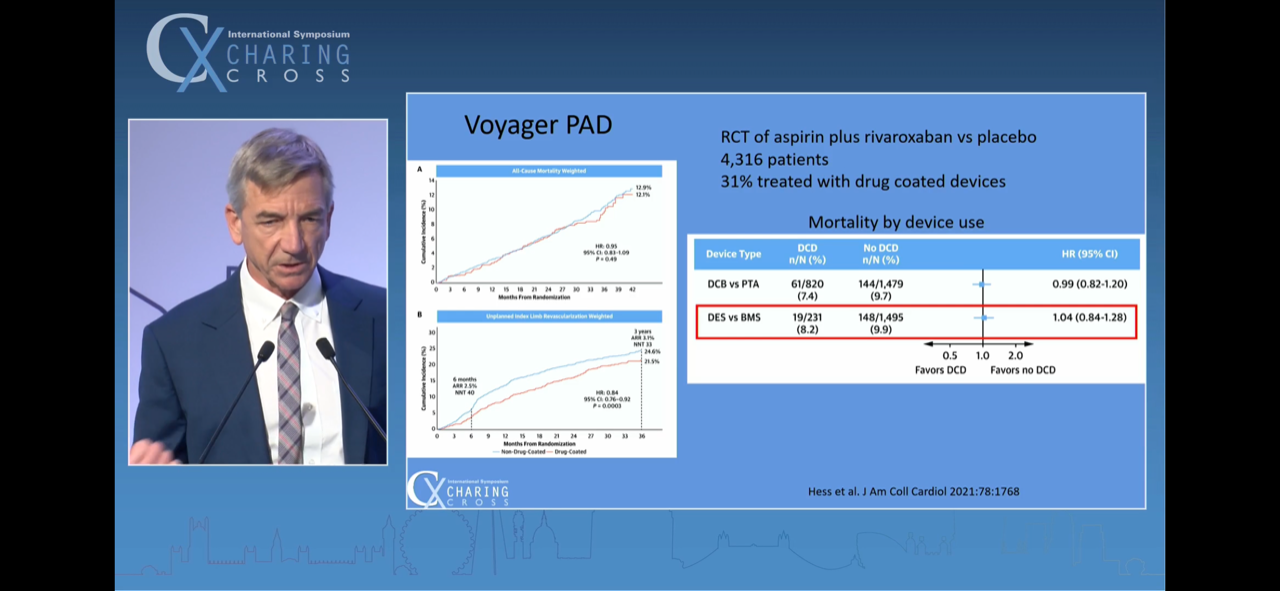
Full data set on VOYAGER PAD - 2.6% absolute risk reduction over 3 years of composite primary endpoint of ALI, Major LL amputation of vascular aetiology, MI, Ischaemic stroke or Cardiovascular death. NNT=39.
The arm that had the benefit of 2.6% was given Aspirin 75 + Rivaroxaban 2.5 BD daily. The other arm had Aspirin and Placebo.
The benefit in the surgical subgroup analysis of VOYAGER PAD was even more pronounced.
4.2% absolute risk reduction over 3 years of composite primary endpoint of ALI, Major LL amputation of vascular aetiology, MI, Ischaemic stroke or Cardiovascular death. NNT=24.
The surgical revascularisation sub-group had only open surgery, not endovascular recanalisation.
The Aspirin + low dose Riva benefit was maintained across both conduit types, although vein fared better.
TADV - deep venous arterialisation for no hope CLTI. Talk by Miguel Monteiro-Baker
Combining two talks in this section.
Firstly, a descriptive talk on use of LIMFLOW to arterialise the pedal venous arch in CLTI patients with no conventional revascularisation options by Miguel Montero-Baker.
Latterly, a few slides from Steven Kum’s talk on the LIMFLOW device evolved technology.
PROMISE and ALPS are registries of deep venous arterialisation for CLTI. Miguel says PROMISE 2 is with the FDA at present. He emphasises that all patients in both registries were those with CLTI facing major amputation and highlights the 24 month 75% limb salvage rate in that context.
Miguel (and later Peter Schneider, during the discussion) emphasised a high MAC score (medial arterial calcification, as per Roberto Ferraresi’s work) to be instrumental in flagging up CLTI patients at high risk of being no-hopers for conventional revasc.
The AV fistula creation (percutaneously) needs the LIMFLOW device. A needle is pushed through from the artery (with IVUS guidance) into the vein, and retrieved to have a through and through wire. Valvulotomy, and covered stent.
There was a great deal of discussion about this approach. The two main issues are (a) getting the valves done and (b) actually perfusing into the tissue. Peter Schneider made some very useful comments. Apparently the foot looks dreadful for the first week. And it takes about 3 weeks for the wound to start showing any improvement - presumably because it takes that long for the effect of the AVF to start telling on the tissue. So Schneider emphasised that this isn’t a strategy appropriate for a large wound with rapidly progressing infection.
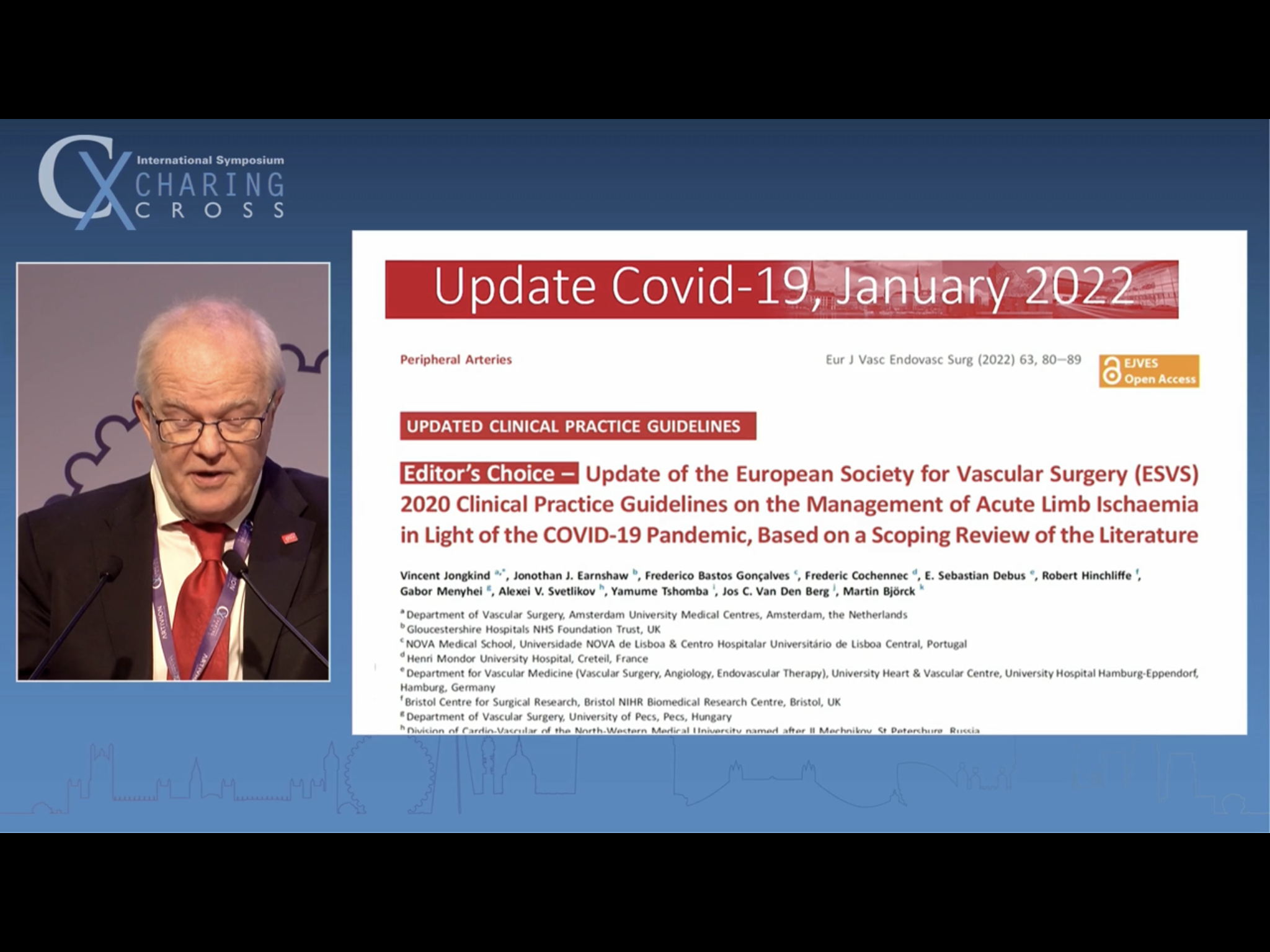
Post CV19 update ALI guidelines ESVS 2020
Talk by Martin Bjorck describing a few post CV19 modifications to the 2020 ESVS guidelines on Rx of ALI
One of the things Martin mentioned was that there is an understanding of greater bleeding risk with full anticoagulation in CV19 - he alluded to a study from Brazil.
Having mentioned that the original and update papers are free to access online, Martin finished with this slide about the war crimes in Ukraine
Hurting Legs - Prof Mike Edmonds
Excellent talk by Prof Edmonds. Highlights: (1) Inequities (2) 6 subtle types of clinical progression (3) Speed to intervention [revasc] is what makes all the difference.
(the amputation rate per se is static because the number of diabetics is also on the rise)
Mike said there are 13 CCGs considered particularly bad in terms of their poor lower limb amputation inequity.
This is true and, pun unintended, very timely, at this juncture when the Provision of Vascular Services document from March 2019 is being incorporated by the NHS in 2022 as a CQUIN to encourage revascularisation within 5 days (IP) to 14 days (OP).
Brilliant! Hadn’t thought of CLTI in these terms but Prof Edmonds has this spot on. He went on to talk about each of the 6 aetiologies has subtly different clinical progression.
- another excellent summary of 6! 6 things to target!
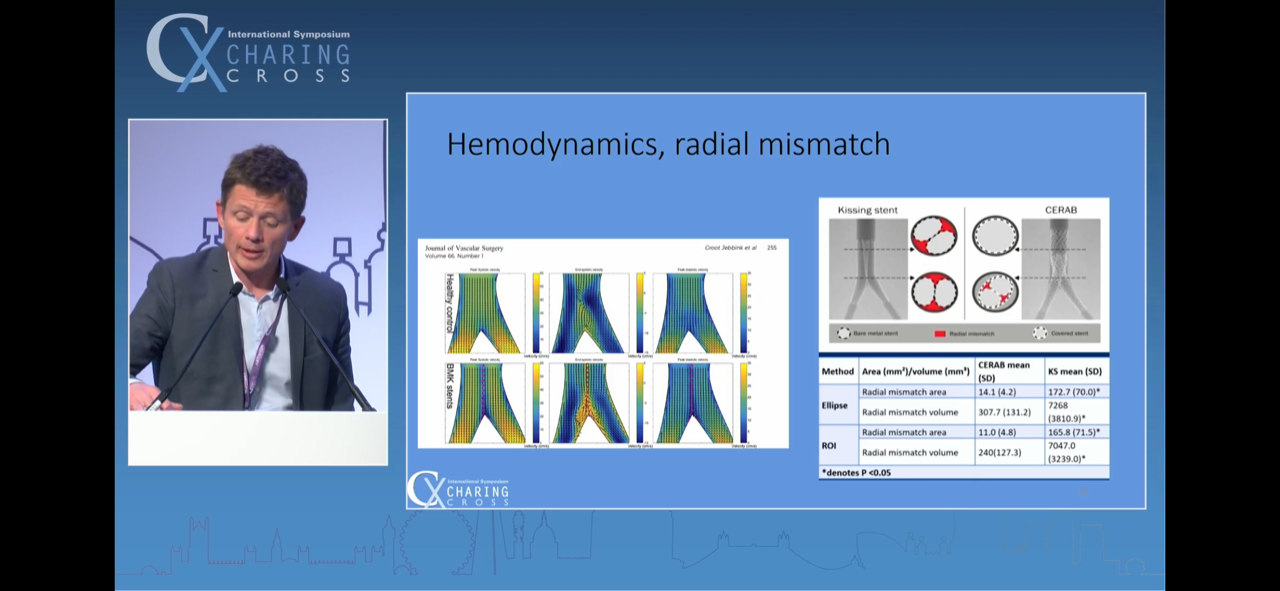
Budtz-Lilly on AIOD recanalisation technique.
A technique presentation on CERAB by Jakob Budtz-Lilly, who I remember as winner of the 2nd ESVS video contest about a decade ago. His pique at the scant 5 minutes accorded for his talk was laid bare. Slick! Good references on last slide.
A 3 word summary of his talk: VBX is king.
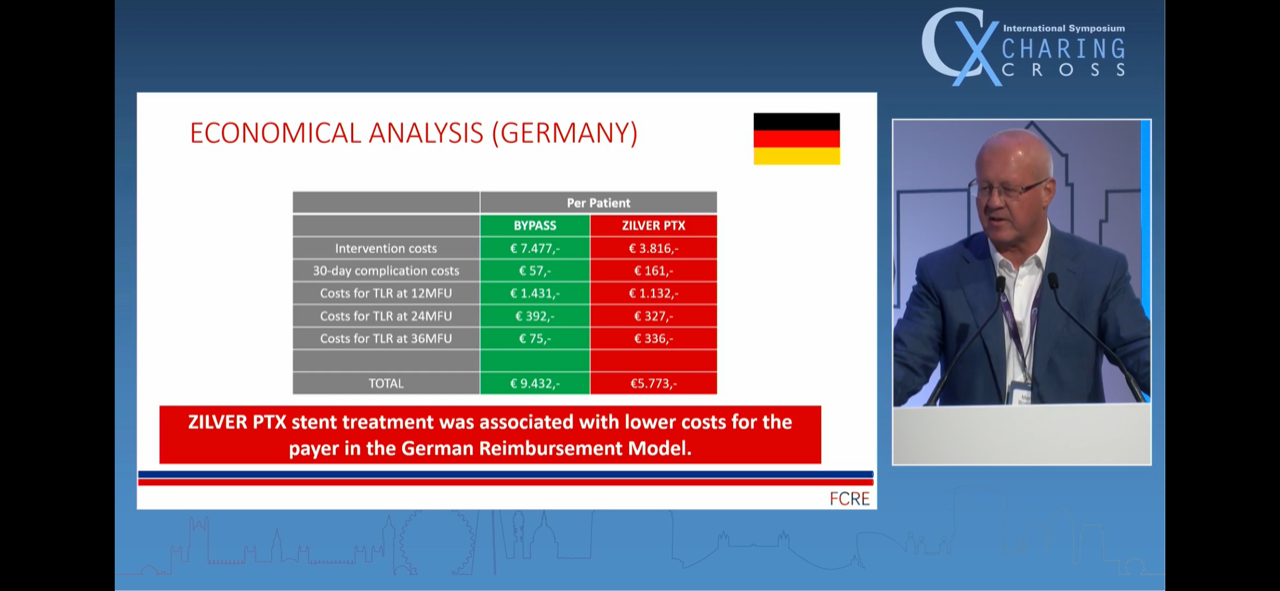
Joshing Zeller - cost of SFA stent vs. Fem Pop bypass
A rather colourful exchange between Alun Davies and Thomas Zeller concluded this talk by the latter, which appeared to demonstrate that the economic cost of a bypass was substantially greater than that of an SFA stent - including secondary intervention expenses - in both Germany and the USA. Words were had - Roger Greenhalgh couldn't help muck in too - about whether surgeons lie about their length of stay.
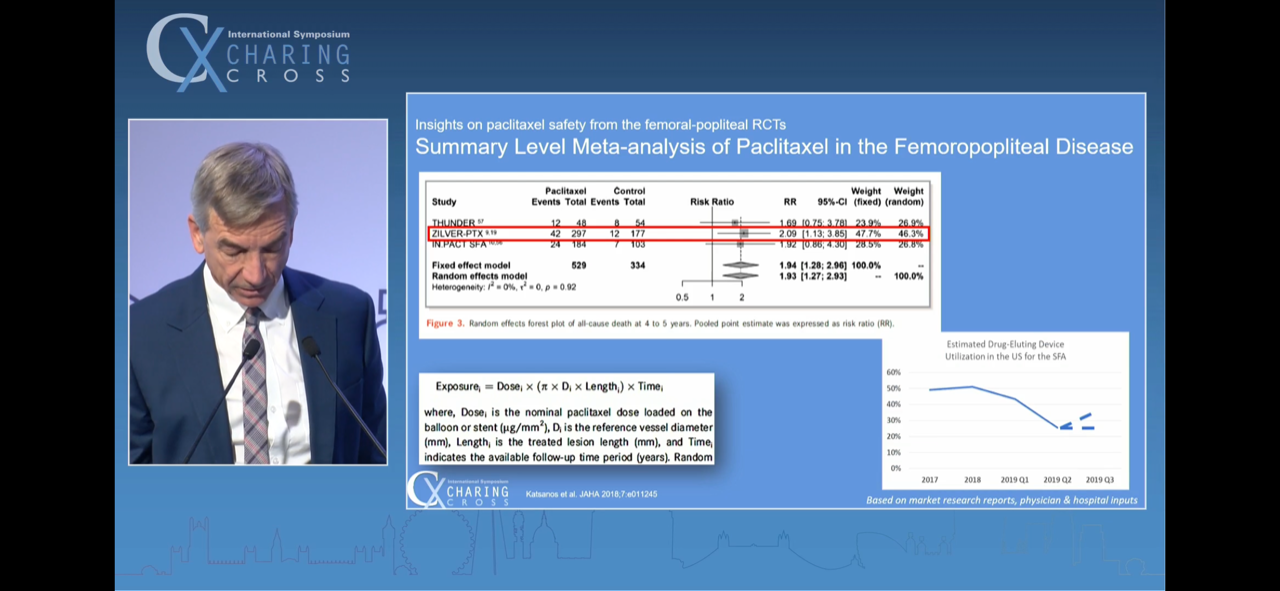
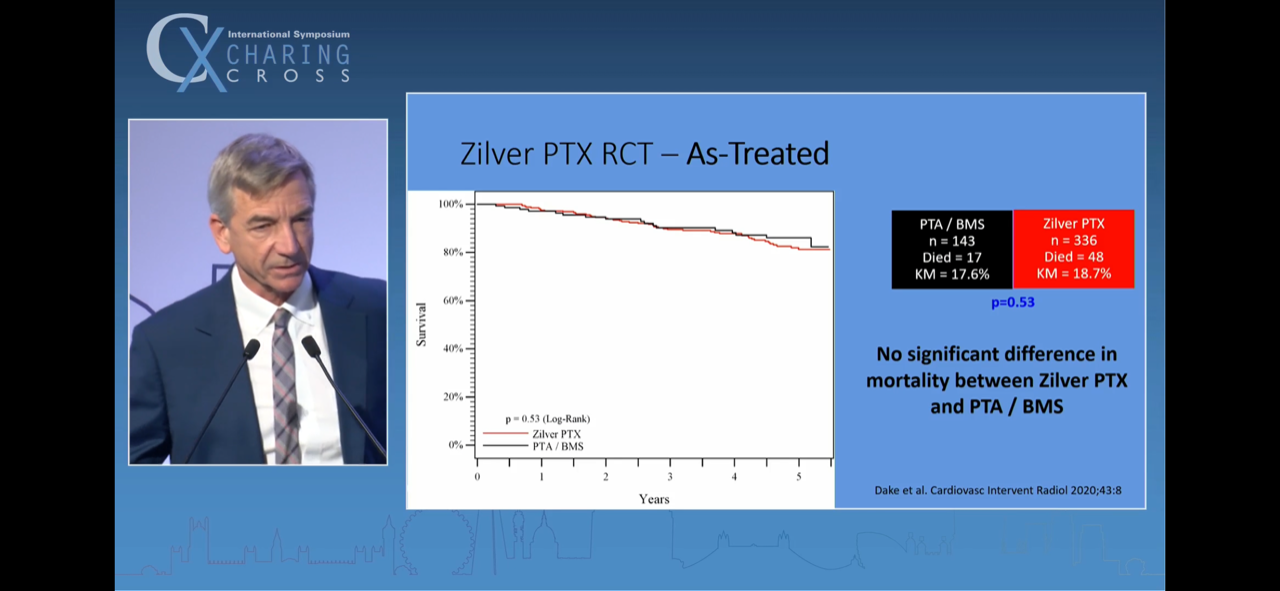
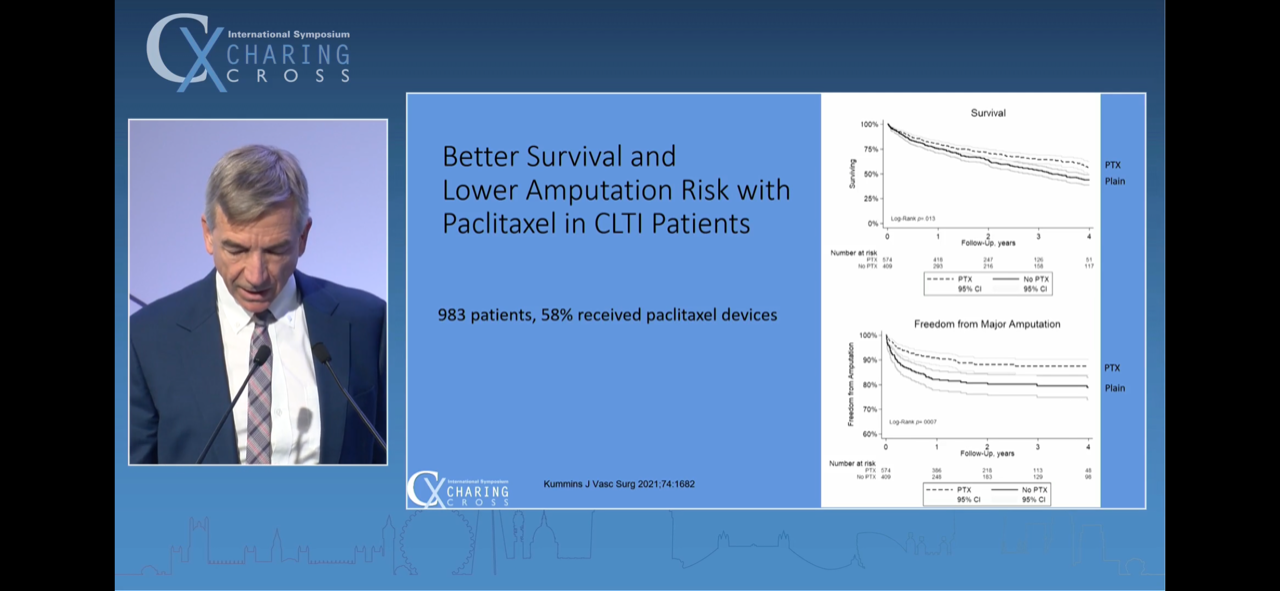
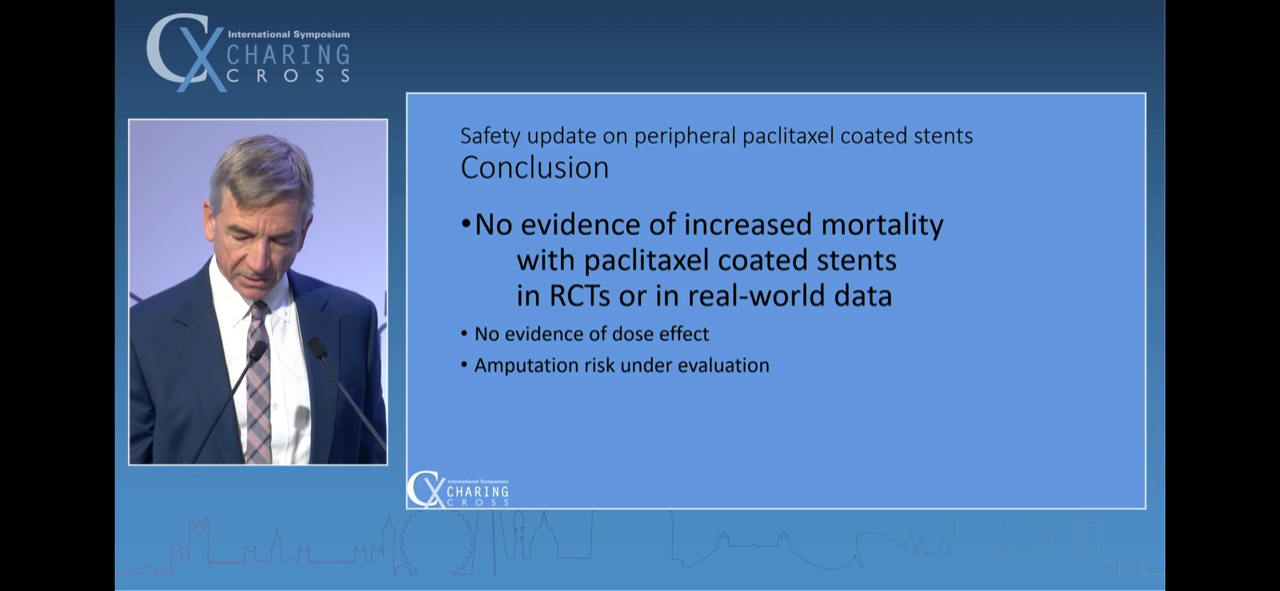
Peter Schneider - The data negates a mortality spike with paclitaxel DCB.
The seminal talk for me from day one of Charing Cross 2022. Schneider spoke eloquently about 3 aspects.
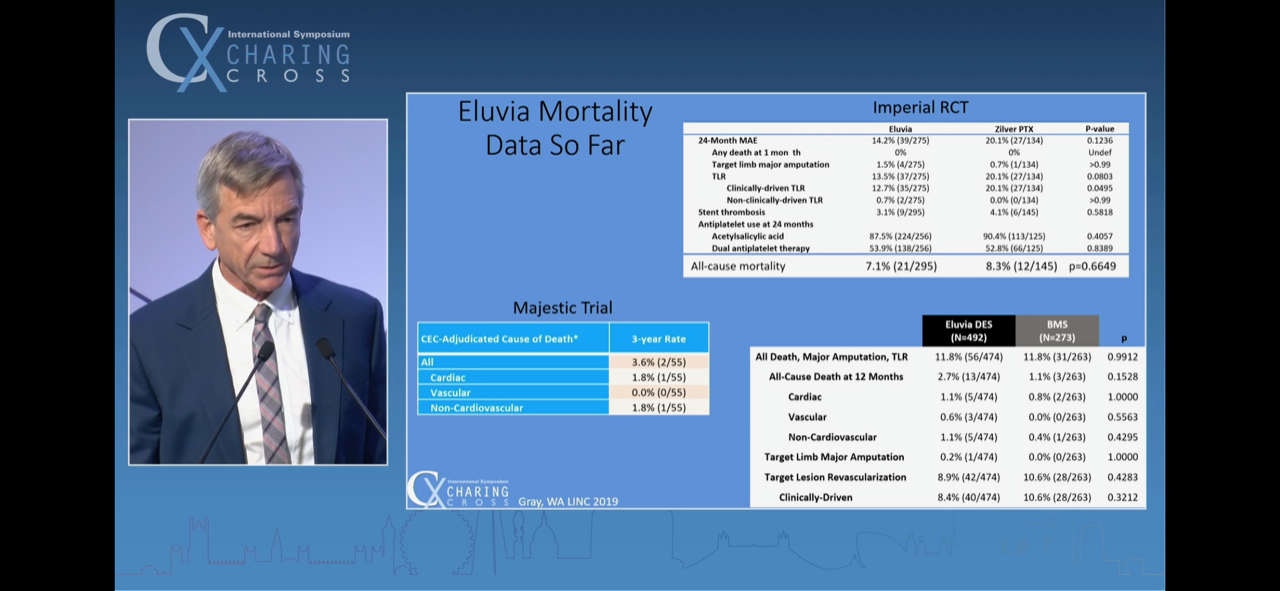
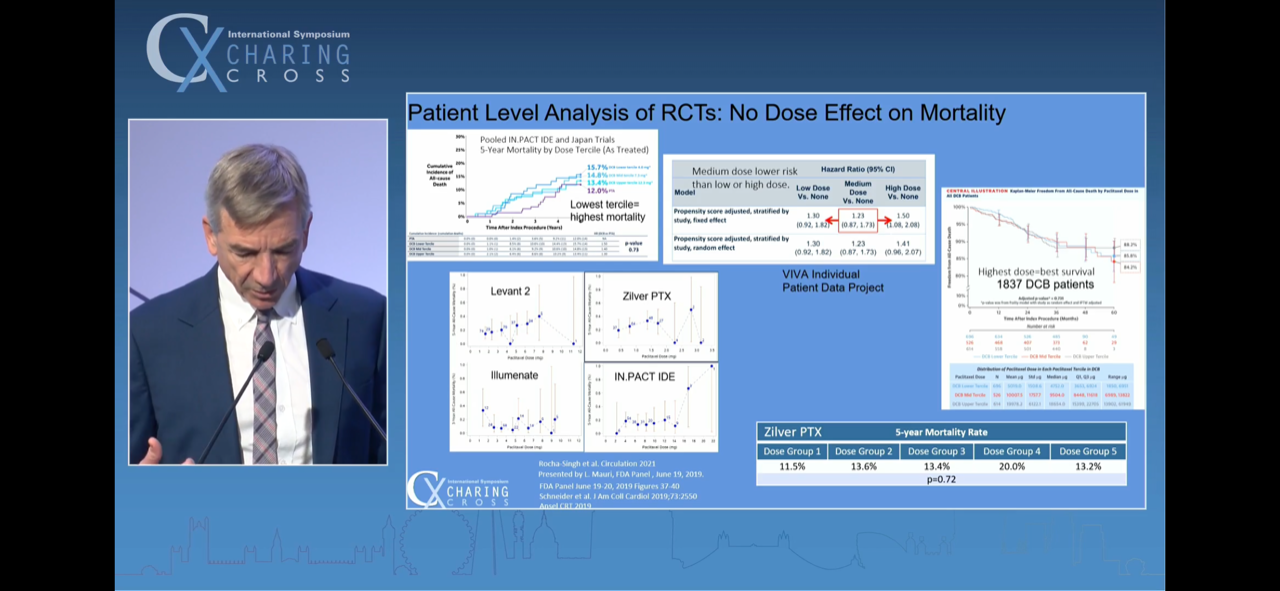
1 - The bulk of Katsanos’ 2018 paper data (50% of it) was from the ZILVER PTX study. In that RCT, a substantial number of patients who were not randomised to DCB on the Intention To Treat analysis were in fact eventually treated with paclitaxel. Upon analysing the patient level ‘actual treatment’ data, there is no difference in mortality between the DCB and non DCB angioplasty groups.
2 - Subsequent registry data, including SWEDE PAD and a subgroup analysis of VOYAGER PAD studies, are not substantiating any mortality spike with paclitaxel
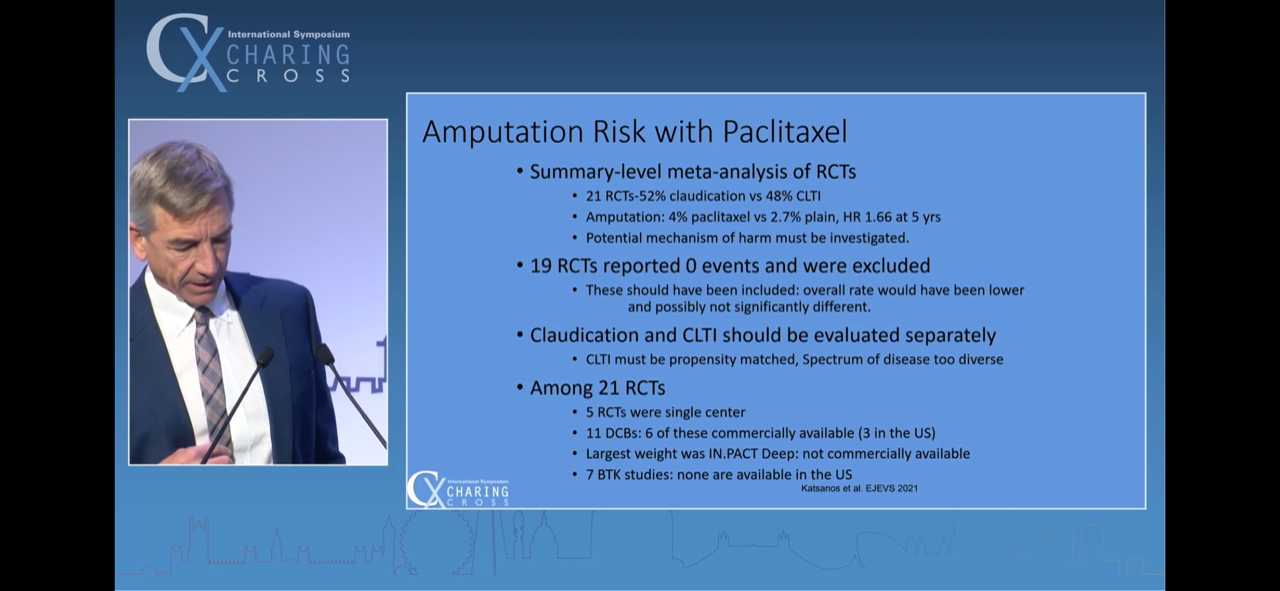
3 - All patient-level data meta-analysis, as opposed to summary-level data meta-analysis, is not reflecting a mortality spike with paclitaxel. Schneider on his penultimate slide was highly critical of and bemused by the fresh MHRA guidance that has come out in the UK in March 2022, stating that DCB shouldn't be used in claudicants, seeing as much of the data in the Katsanos trial was from IC pts.
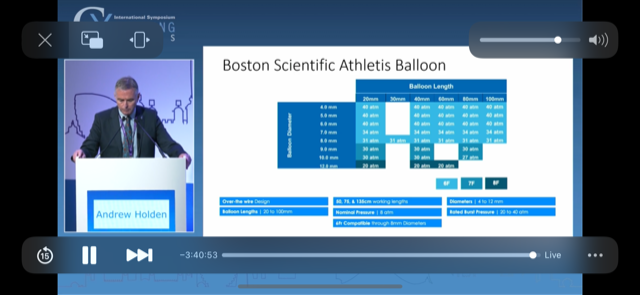
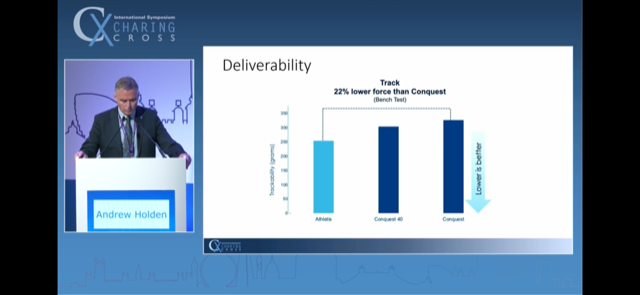
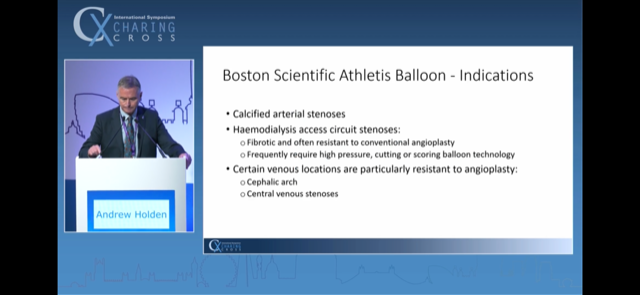
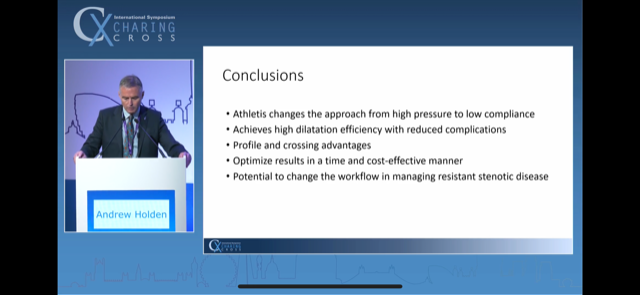
Athletis - new non-compliant balloon. An Andrew Holden 'first-in-human'.
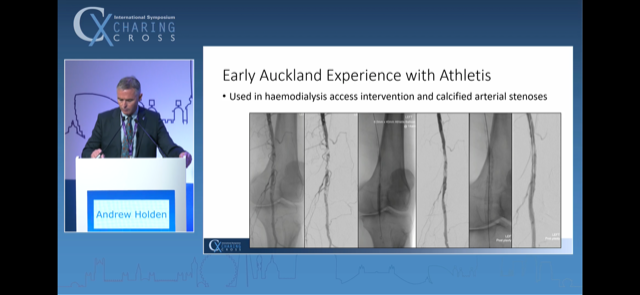
Non compliant balloon that achieves the radial force at about 8 mm that would otherwise require use of a 30 mm Hg high pressure balloon. Boston Scientific. New.
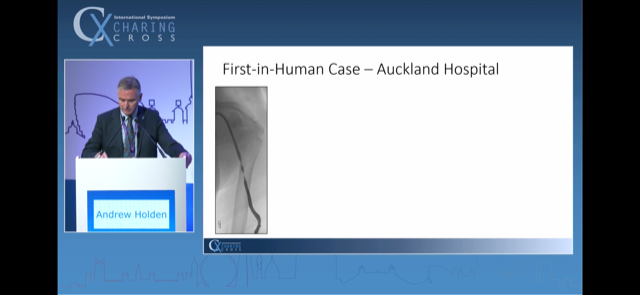
Dr Holden went on to describe the first in human case - a BCAVF that had required 30mm Hg dilatation of stenosis at the index intervention (with severe pain) and which had now recurred.
The balloon has applicability in the calcific LL stenotic disease segments too. In this example it was used and then the residual was stented with a Supera.
Talks about the CV19 impact upon vascular surgery
I watched 5 talks in detail. One was about pathophysiology of CV19 thrombosis. One about ALI. Three were about the impact of Covid-19 upon vascular training; 1 from Rouleaux for the UK, 1 from the ESVS by EVST and 1 from the SVS. There was nothing particularly new in the thrombosis related talks.
The UK trainees apparently filled their boots with emergency work instead of elective; the European trainees in their formative years during CV19 apparently have suffered with no means of reparation in sight; and the American trainees statedly evolved amazing online teaching mechanisms for themselves by March 2020 and rolled with it.
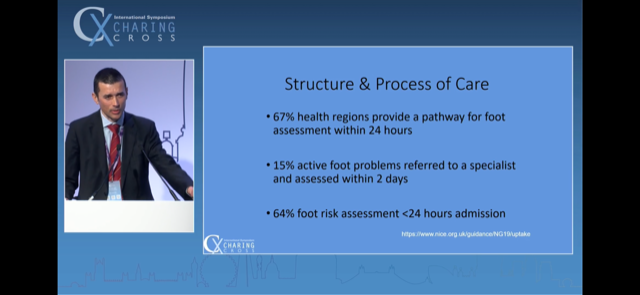
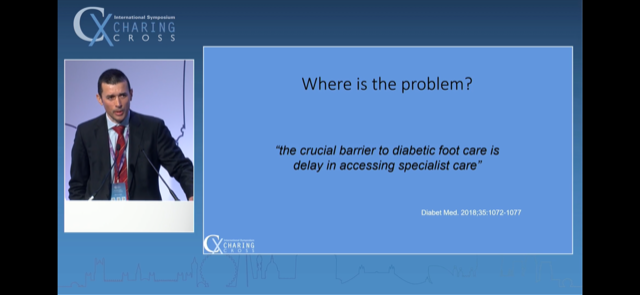
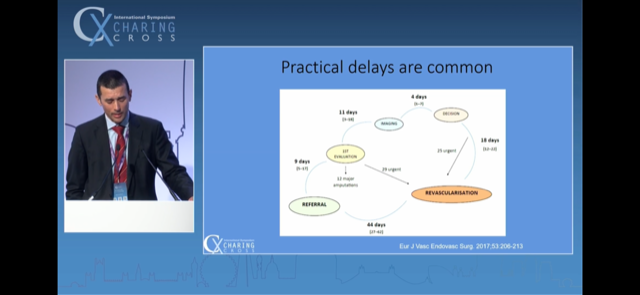
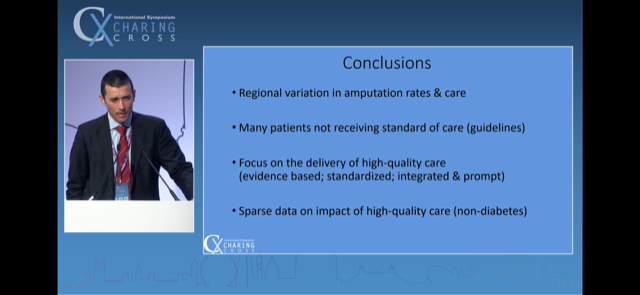
Rob Hinchliffe on lower limb / CLTI care delivery in the UK
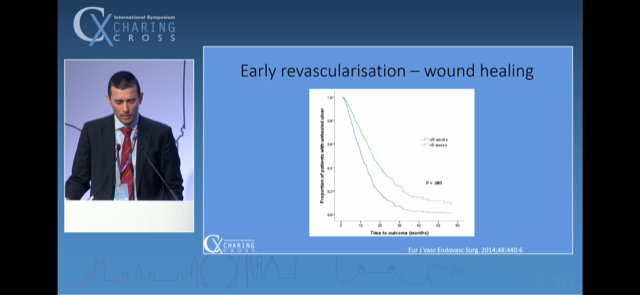
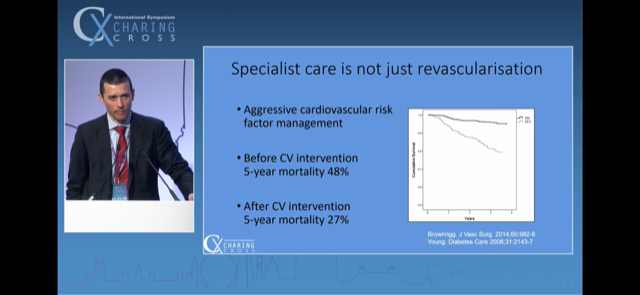
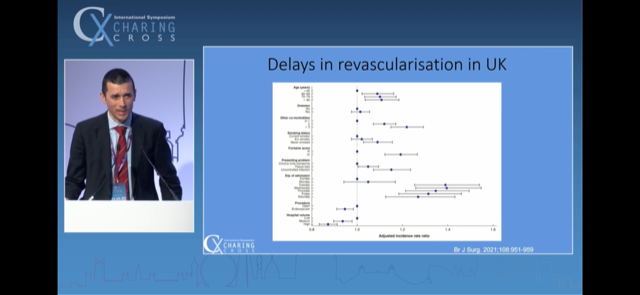
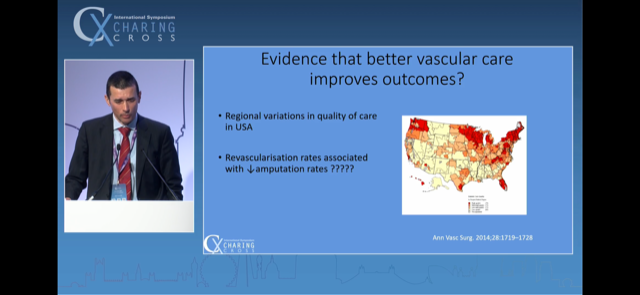
Very slick. Highlighted that time-to-specialist-intervention is variable and is the main bottleneck. Detailed a number of important lower limb revasc. papers clearly along his slides - which exam going trainees in particular will find particularly valuable.
Ref above is the NICE NG19 guidance website
Ref above - Diabet Med. 2018;35:1072-1077
Ref above - EJVES 2017;53:206-213
Ref above - EJVES 2014;48:440-6
Refs above. Brownrigg. JVS. 2014;60:982-6 and Young. Diabetes Care 2008;31:2143-7
BJS 2021;108:951-959
Annals Vasc Surg. 2014;28:1719-28.
Did take one contentious stand in my view - that complex “outlandish” salvage manoeuvres had no role, because the greater good would come from doing only tried and tested stuff, and doing it in time.